Safety pharmacology endpoints may be incorporated into general toxicity studies in order to reduce animal use. This practice is routine for biologics.
May include non-animal methods.
May be based on a risk assessment that includes information from biodistribution data for radiopharmaceuticals.
In vitro preparations can be used as test systems (e.g., cell cultures, receptors, ion channels, transporters and enzymes). In vitro systems can be used in supportive studies (e.g., to obtain a profile of the activity of the substance or to investigate the mechanism of effects observed in vivo).
An appropriately qualified proarrhythmia risk prediction model could be used according to its context of use to assess the possibility of torsades de pointes (TdP) in humans.
The analysis of QTc interval together with adequate pharmacokinetic sampling makes it possible to perform dedicated exposure-response modeling similar to concentration-QT analysis for clinical QT studies.
Different models, including in silico, in vitro, ex vivo and in vivo models, have the potential to be used as part of an integrated risk assessment strategy to evaluate the proarrhythmic risk of QT-prolonging pharmaceuticals in humans.
If both rodents and non-rodents (nonhuman primates or NHPs) are pharmacologically relevant, use a single species if no differences are noted in short-term studies.
Use the phylogenetically lower species.
Chronic toxicology studies can be six months long.
Information on recovery can be obtained by an understanding that the particular effect observed is generally reversible/nonreversible; thus, inclusion of recovery animals is not necessarily warranted. When warranted, they only need to be included in one toxicology study.
Small molecule drugs and biologics: chronic toxicity is of three-month duration. When the investigational pharmaceutical extends survival or lessens the severity or the frequency of a debilitating event, toxicology studies of six to nine months duration are generally not warranted.
For an individualized antisense oligonucleotide, a single three-month toxicity study is considered adequate to assess safety for initiating human dosing, dose escalation, and chronic treatment.
In general, toxicology studies investigating the safety of combinations of pharmaceuticals intended to treat patients with advanced cancer are not warranted.
If sufficient clinical data (e.g., a completed phase 1 or a monotherapy phase within phase 1) are available with the individual pharmaceuticals, additional nonclinical toxicology data may not be warranted. A rationale to support the combination should be provided, which can include in vitro or in vivo pharmacology data or a literature assessment.
If there is no or very limited human safety data for one of the combination components, a nonclinical pharmacology study of the combination should be considered, in addition to the toxicology studies with the single agents.
For pharmaceuticals that are pharmacologically inactive in animal species, assessment of combination can be based on relevant in vitro tests and/or a mechanistic understanding of target biology.
Carcinogenicity studies are not generally needed for endogenous substances given as replacement therapy (i.e., physiological levels).
When a drug is unequivocally genotoxic, a carcinogenicity study is not warranted as the drug is presumed to be trans-species carcinogen.
Pharmaceuticals administered infrequently or for short duration of exposure (e.g., anesthetics and radiolabeled imaging agents) do not need carcinogenicity studies unless there is cause for concern.
The two-year study in rats may be substituted with a weight of evidence (WoE) risk assessment. A WoE assessment may inform whether a two-year rat study is needed.
An alternative to a two-year mouse study may be a six-month study in transgenic strains of mice, which typically employ fewer animals.
Animal carcinogenicity studies are generally not warranted when any of these applies:
Carcinogenicity signals have been identified in general toxicology studies or in humans; the drug is a genotoxic cytotoxic agent; a WoE risk assessment was conducted that can determine the outcome; product-specific agreement (see the guidance for GnRH analogues in prostate cancer).
When an animal study is warranted, it could be conducted postapproval, as appropriate (e.g., when clinical development is short and carcinogenicity studies would delay product approval).
Studies may be submitted at the time of marketing application in certain circumstances.
A number of alternative in vitro, ex vivo, and nonmammalian in vivo assays (alternative assays) have been developed to detect potential hazards to embryo-fetal development. The use of alternative assays for these purposes is encouraged.
If alternative approaches are used for embryofetal development studies, multiple alternative assays used within a tiered or battery approach should provide a level of confidence for human safety assurance at least equivalent to that provided by the current testing paradigms.
If in vivo studies are used, use of the same species and strain as that in already completed toxicity studies can eliminate the need to use additional animals or conduct additional studies.
Combination studies can be employed to assess all relevant stages of the reproductive process using fewer animals.
Embryofetal developmental studies are not considered essential for pharmaceuticals that are genotoxic and target rapidly dividing cells or belong to a class that has been well characterized as causing developmental toxicity.
In cases where an embryofetal developmental toxicity study (including pilot non-GLP study) is positive for embryofetal lethality or teratogenicity, a confirmatory study in a second species is usually not warranted.
A WoE approach showing potential for reproductive toxicity may eliminate the need to conduct a dedicated study.
A WoE risk assessment can be used for small molecule drugs and biopharmaceuticals. The WoE can include a literature assessment of target biology, use of alternative assays such as fit-for-purpose in vitro or ex vivo, or nonmammalian in vivo assays.
When the product is active in rodents and rabbits, sponsors should use these species (instead of NHPs) for EFD assessment. When a study is positive, a study in the second species is not warranted.
DART studies may not be warranted if the WoE risk assessment suggests an adverse effect on fertility or pregnancy.
If a biologic is only active in NHPs, conduct a single enhanced pre-/postnatal development study. Additionally, fertility can be assessed by evaluation of the reproductive organs in general toxicology studies rather than a standalone study.
If clinical studies include sufficient precautions to prevent pregnancy, studies may be conducted during phase 3.
An alternative model can be used in place of NHPs if appropriate scientific justification is provided.
Juvenile animal studies (JAS) should only be conducted when human adult data and data from general animal toxicology studies are not adequate for assessing risk to the intended pediatric population.
WoE-based decisions should be made. JAS are not considered important to support short-term pharmacokinetic studies in pediatric populations, and a WoE-based decision should be made. Changing the design of a traditional nonclinical program can address pediatric concerns (e.g., dosing at a younger age in repeat-dose toxicity). If JAS are conducted, combine assessment of endpoints in the same subset of animals.
Studies in juvenile animals are not usually conducted to support the inclusion of pediatric populations for the treatment of cancer.
JAS are not needed to initiate clinical trials in pediatric populations when clinical data in adults are available.
Immunotoxicity could be addressed through in vitro assays, a WoE assessment, or by adding endpoints into the design of general toxicity or proof-of-concept studies. Stand-alone animal immunotoxicity studies should only be conducted if the WoE from the general animal toxicology studies, knowledge of the target biology and/or pharmacokinetic/pharmacodynamic data suggest a risk that should be better characterized.
For most anticancer pharmaceuticals, the design components of the general toxicology studies are considered sufficient to evaluate the immunotoxic potential and support marketing.
For pharmaceuticals activating the immune system, the sponsor can consider additional endpoints (such as immunophenotyping by flow cytometry) in the toxicology or proof-of-concept study design.
To assess immune activation, an appropriate assay to be considered. Examples include cytokine release assay, antibody-dependent cellular cytotoxicity and complement-dependent cytotoxicity assays.
Typically non-animal evaluations.
A risk assessment should be considered, such as photochemical properties and findings from nonclinical and clinical studies.
Examples (not all inclusive):
For oncology therapeutic radiopharmaceuticals when there is experience with the radionuclide or the ligand components of the radiopharmaceutical being developed, the nonclinical program can be abbreviated as needed, and the FIH dose can be based on clinical data.
When an animal dosimetry study is needed, the sponsor should evaluate radioactivity in organs over time post-administration. Duration of data collection can be adjusted as needed or alternative approaches and modeling can be considered.
For certain anticancer biological products, doses given to patients with related/relevant biological products may inform on FIH dosing.
A 2022 research project showed that for the CD3 bispecific products examined, absence of chronic (i.e., three-month) toxicology studies did not have adverse regulatory impact. When three-month studies were conducted, they were not informative; toxicities were predicted based on the available information (pharmacology and short-term toxicology, target biology, and phase 1 human data). Thus, a WoE assessment may predict the outcome of chronic dosing.
Data collected (2017) shows common toxicities in animals from CD3 bispecifics (e.g., cytokine release syndrome and inflammatory response) and challenges associated with conducting three-month toxicology (e.g., anti-drug antibody formation, confounding the results).
Data collected for ADCs with cytotoxic payloads indicate that toxicities of these products are mainly from the payload. Toxicity profiles of ADCs that contain the same payload were comparable in animals, independent of the monoclonal antibody moiety. Thus, streamlined approaches reducing use of NHPs may be applicable for certain ADCs.
Studies of the linker or the monoclonal antibody alone are not warranted.
Flexibility and adherence to 3Rs discussed in several FDA publications (e.g., reprotoxicity, safety pharmacology, acute toxicity, local tolerance, juvenile animal toxicity, immunotoxicity, phototoxicity, and liver toxicity), and data-driven external publications.
For oncology indications, sponsors can choose to conduct the three-month toxicology study before initiating a phase 1 human study, in which case a one-month toxicology study (generally warranted to support a phase 1 study) won’t be needed.

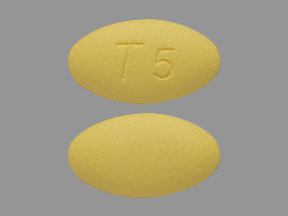
 Our Pill Pass® Drug List is only $6.99 or less and Shipping is FREE!
Our Pill Pass® Drug List is only $6.99 or less and Shipping is FREE!