Delivery Method: VIA UPS Reference #: 320-26-12 Product: Drugs Recipient:
Recipient Name
Mr. Allan Oberman
Recipient Title
President & Chief Executive Officer
Apotex Inc.
150 Signet Drive
Toronto ON M9L 1T9
Canada
Issuing Office: Center for Drug Evaluation and Research (CDER)
United States
Warning Letter 320-26-12
October 31, 2025
Dear Mr. Oberman:
The United States Food and Drug Administration (FDA) inspected your drug manufacturing facility, Apotex Inc., FEI 3001617666, at 380 Elgin Mills Road East, Richmond Hill, from April 28 to May 9, 2025.
This warning letter summarizes significant violations of Current Good Manufacturing Practice (CGMP) regulations for finished pharmaceuticals. See Title 21 Code of Federal Regulations (CFR), parts 210 and 211 (21 CFR parts 210 and 211).
Because your methods, facilities, or controls for manufacturing, processing, packing, or holding do not conform to CGMP, your drug products are adulterated within the meaning of section 501(a)(2)(B) of the Federal Food, Drug, and Cosmetic Act (FD&C Act), 21 U.S.C. 351(a)(2)(B).
We reviewed your June 2, 2025, response to our Form FDA 483 in detail and acknowledge receipt of your subsequent correspondence.
During our inspection, our investigators observed specific violations including, but not limited to, the following.
1. Your firm failed to thoroughly investigate any unexplained discrepancy or failure of a batch or any of its components to meet any of its specifications, whether or not the batch has already been distributed (21 CFR 211.192).
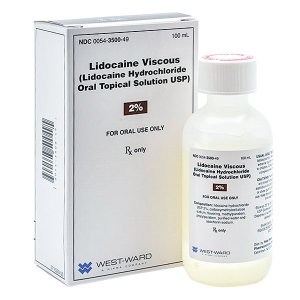
Your firm failed to conduct adequate investigations for your (b)(4) solutions, (b)(4) solutions, and (b)(4) spray drug products distributed to the U.S. market. For example, you did not properly investigate critical equipment failures and container-closure integrity issues to evaluate root causes or assess impact on other potentially affected batches in a timely manner.
Between September 2023 and April 2025, your firm failed to adequately investigate at least eight failures during (b)(4) leak testing. (b)(4) leak tests are critical for verifying the integrity of your (b)(4). Production personnel repeatedly performed leak testing until they obtained passing results instead of investigating the root cause of identified failures. Consequently, for more than a year, production personnel used the (b)(4) to aseptically fill (b)(4) products without adequately addressing the uncertainty of (b)(4) integrity.
Moreover, at the time of our inspection, while you were investigating this issue, more than 30 individual areas of the (b)(4) system were found leaking, including multiple (b)(4) used to introduce sterile components.
Notably, another regulator identified (b)(4) integrity issues prior to our inspection.
Also, your firm failed to thoroughly review discrepancies and assess the impact on distributed batches associated with identified failures of container-closure integrity of (b)(4) solution. On June 17, 2024, your firm found (b)(4) residue under the closure of a stability sample of (b)(4) solution. Your investigation determined the root cause was due to the product formulation being incompatible with the container-closure cap liner and inadequate cap sealing. This incompatibility led to corrosion of the closure liner and product leakage. Although you determined the risk to be “Undesirable / High risk,” no market action was taken at the time for products in U.S. distribution.
In addition, your firm did not sufficiently investigate recurring incidents in which individual units of multiple products experienced excessive (b)(4) loss when tested as part of your stability program.
In your response, you indicate that you have implemented corrective action and preventive action (CAPA) to address specific observations cited during the inspection, including revisions to your standard operating procedures (SOP). You also commit to have an independent consultant assess your post-market data, and retrospectively review deviations and your escalation process. Additionally, you commit to document (b)(4) leak test results in the batch record and require quality unit review of all such leak tests.
We acknowledge you have subsequently recalled some of these products, but your response is inadequate because you do not adequately address your failure to identify and correct these issues in a timely manner. The reactive approach after our inspection does not sufficiently explain how you will improve your quality system to ensure comprehensive investigations of discrepancies that could impact product quality and implementation of timely, appropriate actions.
The quality unit has the responsibility to ensure that investigations are scientifically sound, consider all available data, expand to include all potentially affected drug products, and result in timely, appropriate actions to protect public health.
In response to this letter, provide:
- A comprehensive, independent assessment of your overall system for investigating deviations, discrepancies, complaints, out-of-specification (OOS) results, and failures. Provide a detailed action plan to remediate this system. Your action plan should include, but not be limited to, significant improvements in investigation competencies, scope determination, root cause evaluation, CAPA effectiveness, quality unit oversight, and written procedures. Address how your firm will ensure all phases of investigations are appropriately conducted.
- An independent assessment and remediation plan for your CAPA program. Provide a report that evaluates whether the program includes effective root cause analysis, ensures CAPA effectiveness, analyzes investigation trends, improves the CAPA program when needed, implements final quality unit decisions, and is fully supported by executive management.
2. Your firm failed to establish and follow appropriate written procedures that are designed to prevent microbiological contamination of drug products purporting to be sterile, and that include validation of all aseptic and sterilization processes. Your firm also failed to perform operations within specifically defined areas of adequate size and to have separate or defined areas or such other control systems necessary to prevent contamination or mix-ups in aseptic processing areas (21 CFR 211.113(b) & 211.42(c)(10)).
Cleaning, Decontamination, and Maintenance
You failed to adequately clean, decontaminate, and maintain your (b)(4) used for aseptic drug product manufacturing. For example, our investigator observed multiple instances of deterioration and damage to the (b)(4) used for manufacturing sterile (b)(4) drug products. These instances of deterioration and damage were not adequately addressed through your cleaning, decontamination, and maintenance programs. For example, our investigator observed:
- discolored (b)(4) gloves
- excess sealant adjacent to the (b)(4)
- various discolorations of undetermined origin (e.g., possibly dried drug product residue) on interior equipment surfaces
- a notably discolored plastic utensil within the (b)(4) environment
- deteriorated gasket seals
Additionally, your personnel failed to follow established (b)(4) decontamination procedures. Numerous creases were observed in (b)(4) glove (b)(4) during decontamination cycles, despite your procedure requiring (b)(4) to be “free of creases.” Incomplete exposure of interior surfaces to (b)(4) compromises decontamination effectiveness and places the (b)(4) environment at risk.
Regarding maintenance, our investigator observed multiple instances of tape applied to multiple “false covers” which are used to maintain a sealed environment during the (b)(4) decontamination cycle. The use of tape is an insanitary practice and your firm could not explain the presence of this tape. Maintenance and change management procedures should prevent such practices that may compromise equipment or introduce contamination risks.
Your preventive maintenance schedules lack timeframes for critical equipment, such as, gaskets on (b)(4) gloves. It is unacceptable to only belatedly change critical equipment (e.g., gloves, gaskets) when a leak occurs. This solely reactive approach to maintenance fails to safeguard against a critical failure mode in (b)(4) technology.
The integrity of equipment should receive daily attention through comprehensive preventive maintenance procedures that establish adequate integrity testing, cleaning and disinfection methods, and proactive replacement before breakdown or degradation.
Notably, you experienced (b)(4) glove breach events during the manufacturing of three different batches of (b)(4) drug products, creating a risk of contamination. One of the breach events included a six-millimeter hole that was closed with a “cable tie” after which processing continued. This practice is unacceptable as it does not sufficiently mitigate the breach in (b)(4) associated with a loss of glove integrity. You released these products but later recalled them after our inspection.
Environmental Monitoring
Your environmental monitoring program is deficient as it fails to adequately monitor the aseptic processing line. For example, critical areas within the (b)(4) lack continuous non-viable particle monitoring. Instead, you rely on a single monitoring probe oriented away from critical areas where open processing occurs. Your inadequate and limited monitoring deprive you of sufficient meaningful data for determining risk to product during batch operations.
Your response is inadequate because your CAPA was not timely. You do not propose meaningful corrective actions until a regulatory inspection identified violations that had occurred over an extended period. Furthermore, it is unclear if your CAPA commitment to simply update your written procedure to “minimize creases” in your (b)(4) gloves will ensure surface exposure of all gloves to the (b)(4) decontaminating agent.
Aseptic processes need to be designed to minimize exposure of sterile articles to potential contamination hazards. A suitable monitoring system is critical to maintain appropriate environmental conditions throughout your (b)(4) and cleanrooms. Prompt detection of an emerging problem is essential to preventing contamination of your aseptic production operations. Vigilant and responsive environmental monitoring programs should be designed to provide meaningful information on the state of control of your aseptic processing environment.
See FDA’s guidance document Sterile Drug Products Produced by Aseptic Processing – Current Good Manufacturing Practice to help you meet the CGMP requirements when manufacturing sterile drugs using aseptic processing, at https://www.fda.gov/media/71026/download.
In your response to this letter, provide the following:
- A comprehensive, independent assessment of your change management system. This assessment should include, but not be limited to, your procedure(s) to ensure changes are justified, reviewed, and approved by your quality unit. Your change management program should also include provisions for determining change effectiveness.
- A comprehensive risk assessment of all contamination hazards with respect to your aseptic processes, equipment, and facilities, including an independent assessment that includes, but is not limited to:
o suitability of actual practices based on extensive retrospective review and prospective observation of aseptic processing operations
o deficiencies in production management oversight, and identification of specific improvements to ensure effective and routine supervisory oversight for all batches
o frequency and depth of quality unit oversight (e.g., audit, ad hoc, daily interactions) of aseptic processing and its support operations
o adequacy of written procedures - Your CAPA plan to implement routine, vigilant operations management oversight of facilities and equipment. This plan should ensure, among other things, prompt detection of equipment/facilities performance issues, effective execution of repairs, adherence to appropriate preventive maintenance schedules, timely technological upgrades to the equipment/facility infrastructure, and improved systems for ongoing management review. Your plan should also ensure that appropriate actions are taken throughout the company network.
3. Your firm failed to clean, maintain, and, as appropriate for the nature of the drug, sanitize and/or sterilize equipment and utensils at appropriate intervals to prevent malfunctions or contamination that would alter the safety, identity, strength, quality, or purity of the drug product beyond the official or other established requirements (21 CFR 211.67(a)).
You failed to adequately maintain your equipment. For example, during the inspection, our investigators observed white particle buildup on manufacturing equipment surfaces used to produce (b)(4) spray drug products distributed to the U.S. market. They observed that the source of the particles was the (b)(4) which is made of (b)(4). They saw particles along the conveyor that transports container-closure components (e.g., (b)(4)) to the filling operations. You purchased equipment nearly one year before our inspection that included a design upgrade (e.g., (b)(4)) for your existing (b)(4). However, you continued manufacturing using the deteriorating (b)(4) that was actively generating particles. This demonstrates a failure in your maintenance program to implement timely equipment upgrades necessary to correct and prevent contamination hazards.
Your response is reactive and inadequate because your CAPA was not timely. You did not propose meaningful corrective actions until a regulatory inspection identified violations that had occurred over an extended period.
An effective equipment management program requires a proactive lifecycle approach with systematic monitoring, maintenance, and timely replacement to ensure continued process capability. Pharmaceutical quality systems must integrate equipment performance data, maintenance trending, and risk assessment to drive timely CAPA.
In response to this letter, provide:
- A comprehensive, independent retrospective assessment of your cleaning effectiveness to evaluate the scope of cross-contamination hazards. Include the identity of residues, other manufacturing equipment that may have been improperly cleaned, and an assessment whether cross-contaminated products may have been released for distribution. The assessment should identify any inadequacies of cleaning procedures and practices, and encompass each piece of manufacturing equipment used to manufacture more than one product.
Ineffective Quality System
Significant findings in this letter demonstrate that your firm does not operate an effective quality system in accord with CGMP. In addition to the lack of effective management oversight of your production operations, we found your quality unit is not enabled to exercise proper authority and/or has insufficiently implemented its responsibilities. Executive management should immediately and comprehensively assess your company’s global manufacturing operations to ensure that your systems, processes, and products conform to FDA requirements.
See FDA’s guidance document Quality Systems Approach to Pharmaceutical CGMP Regulations for help implementing quality systems and risk management approaches to meet the requirements of CGMP regulations 21 CFR, parts 210 and 211, at https://www.fda.gov/media/71023/download.
Visual Inspection Program
We acknowledge that you are using an independent third-party consultant to evaluate your visual inspection program. The following items should be considered:
- A comprehensive assessment and remediation plan for your visual inspection program to ensure compliance with CGMP. The remediation plan should incorporate U.S. Pharmacopeia (USP) <790> Visible Particulates in Injections and USP <(b)(4) Products-Quality Tests, including container-specific testing protocols (e.g., translucent containers, opaque containers) for each container type. Your strategy should include:
o Implementing 100% visible inspection using enhanced lighting with background contrast methods, as appropriate, for difficult-to-inspect products (DIP) (e.g., translucent containers) that allow visual inspection.
o For drug products that preclude visual inspection (e.g., products packaged in opaque containers), using destructive testing (e.g., subvisible particulate matter) with appropriate, statistically significant sample sizes to test for critical defects.
o Where traditional visual inspection methods cannot be used, establish periodic in-process visible particulate matter testing for both bulk solution and fill/finish operations to ensure process control, and implement enhanced manufacturing controls, including strengthened filtration and environmental controls.
o Develop a product-specific, risk-based visual inspection approach incorporating product knowledge, process experience, deviation investigation analysis, and recall/complaint data to ensure ongoing compliance with USP <790>, USP <(b)(4)>, and CGMP requirements.
Drug Production Suspension and Recall
After the inspection, we acknowledge you temporarily suspended manufacturing and distribution of certain drugs at this facility for the U.S. market, including sterile (b)(4) solution drugs and small volume (b)(4) spray drugs (i.e., (b)(4) spray), while CAPA were being identified and implemented.
We also acknowledge, based on your review you initiated several voluntary recalls:
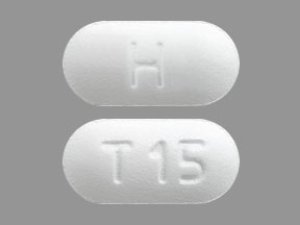
- On May 28, 2025, you voluntarily recalled azelastine HCl ophthalmic solution (batch VD1654), ketorolac tromethamine ophthalmic solution (batch TZ1236), and brimonidine tartrate/timolol maleate ophthalmic solution (batch VC6058) due to (b)(4) glove breach events that occurred during manufacturing.
- On May 28, 2025, you voluntarily recalled lacosamide oral solution, batch TZ5589 due to product leakage.
Conclusion
The violations cited in this letter are not intended to be an all-inclusive list of violations that exist at your facility. You are responsible for investigating and determining the causes of any violations and for preventing their recurrence or the occurrence of other violations.
If you are considering an action that is likely to lead to a disruption in the supply of drugs produced at your facility, FDA requests that you contact CDER’s Drug Shortages Staff immediately, at drugshortages@fda.hhs.gov, so that FDA can work with you on the most effective way to bring your operations into compliance with the law. Contacting the Drug Shortages Staff also allows you to meet any obligations you may have to report discontinuances or interruptions in your drug manufacture under 21 U.S.C. 356C(b). This also allows FDA to consider, as soon as possible, what actions, if any, may be needed to avoid shortages and protect the health of patients who depend on your products.
Correct any violations promptly. FDA may withhold approval of new applications or supplements listing your firm as a drug manufacturer until any violations are completely addressed and we confirm your compliance with CGMP. We may re-inspect to verify that you have completed corrective actions to any violations.
Failure to address any violations may also result in the FDA refusing admission of articles manufactured at Apotex Inc., 380 Elgin Mills Road East, Richmond Hill, into the United States under section 801(a)(3) of the FD&C Act, 21 U.S.C. 381(a)(3). Articles under this authority that appear to be adulterated may be detained or refused admission, in that the methods and controls used in their manufacture do not appear to conform to CGMP within the meaning of section 501(a)(2)(B) of the FD&C Act, 21 U.S.C. 351(a)(2)(B).
This letter notifies you of our findings and provides you an opportunity to address the above deficiencies. After you receive this letter, respond to this office in writing within 15 working days1. Specify what you have done to address any violations and to prevent their recurrence. In response to this letter, you may provide additional information for our consideration as we continue to assess your activities and practices. If you cannot complete corrective actions within 15 working days, state your reasons for delay and your schedule for completion.
Send your electronic reply to CDER-OC-OMQ-Communications@fda.hhs.gov. Identify your response with FEI 3001617666 and ATTN: William Fowler.
Sincerely,
/S/
Francis Godwin
Director
Office of Manufacturing Quality
Office of Compliance
Center for Drug Evaluation and Research
cc:
Mr. Navid Ghamami
Vice President, Product Supply
Apotex Inc.
380 Elgin Mills Road East
Richmond Hill, Ontario, L4C 5H2
Canada
Kiran Krishnan, PhD
Senior Vice President, Global Regulatory Affairs
Apotex Corp.
2400 North Commerce Parkway, Suite 400
Weston, Florida 33326
_______________
1 Under program enhancements for the Generic Drug User Fee Amendments (GDUFA) reauthorization for fiscal years (FYs) 2023-2027, also known as the GDUFA III Commitment Letter, your facility may be eligible for a Post-Warning Letter Meeting to obtain preliminary feedback from FDA on the adequacy and completeness of your corrective action plans.

 Our Pill Pass® Drug List is only $6.99 or less and Shipping is FREE!
Our Pill Pass® Drug List is only $6.99 or less and Shipping is FREE!