Seniors stricken with diabetes must notify their primary care physicians and their assigned medical specialists about their foot problems, federal agency researchers and medical trade associations say.
The National Institute of Health’s National Institute of Diabetes and Digestive and Kidney Diseases, or NIH-NIDDK, the American Diabetes Association, or ADA, and the American Podiatric Medical Association, or APMA, urge senior diabetics to engage not only their family practice physicians and internal medicine physicians about their foot conditions but also other specialists in their care team such as podiatrists, pharmacists, optometrists, ophthalmologists, dentists and dental hygienists.
Federal agency researchers argue that diabetes, eye care, oral care, foot care and drug management are all connected and the physicians in each medical specialty represented can assist seniors in achieving optimal health by addressing all.
In particular, patients must examine their feet for the most common diabetic issues: neuropathy, vasculopathy, dermatological conditions and musculoskeletal problems.
Four Diabetic Issues
Peripheral sensory neuropathy is characterized by tingling, burning, numbness or the sensation of bugs crawling on skin. Doctors can test seniors for neuropathy using an instrument known as a Semmes-Weinstein 5.07 monofilament.
A description of the instrument and its function appears through a health care provider kit on the NIH’s website patients at http://www.ndep.nih.gov/media/Feet_Kit.pdf
Diabetics with neuropathy are almost two times as likely as those without the condition to suffer from foot ulcers. With patients with both neuropathy and foot deformity, the risk is 12 times higher.
The lifetime odds of developing foot ulcers among diabetes is 15 percent. This condition can be prevented through medical care in primary care clinics and preventive health centers.
Seniors with a history of prior amputation or ulcers have a risk of 36 times greater of enduring more ulcers. The highest risk factors for leg ulcers and amputations are being members of the male gender, the condition of diabetes for more than 10 years, tobacco use and a history of poor blood sugar control or heart or kidney disease.
Vasculopathy involves the cramping of calf muscles when walking, also known as “charley horse,” which requires several rest times or breaks. This condition is caused by an insufficient supply of blood to the area below the knee. It also entails a blockage of the arteries common to the legs of diabetes.
Cramping and aching in the toes at night, also known as “rest pain,” is treated by hanging the feet over the side of the bed and by walking. This condition marks the end of the artery disease that comes before diabetic gangrene.
Research links the loss of sensation or neuropathy to ulcers and other complications but poor blood supply can hamper ulcer healing and can lead to amputations.
Dermatological conditions include corns and calluses of the feet resulting from pressure and shearing of the skin. These conditions come before the breakdown of skin and may cause blisters and ulcers.
Cuts and bruises on the heel or softening by wetness between the toes can place patients in danger of infections. Corns, calluses, toenail deformity and bleeding under the nail can mark the presence of sensory neuropathy. Fungus of the skin or nails can end with bacterial infections.
Musculoskeletal symptoms may lead to structural changes in the diabetic foot along with muscle-tendon imbalances caused by motor neuropathy. These condition include hammertoes, bunions, high-arched foot or flatfloot, which can all lead to focal irritation of the foot in the shoe.
Link Between Diabetes and Foot Health
The first symptoms of the onset of diabetes may emerge with the foot. Foot problems heighten the risk for multiple conditions of diabetes, with lower extremity amputations being the most worrisome.
In 1997, federal hospital discharge data found that diabetes was connected to 87,720 amputations in the United States or 67 percent of the incidence of this surgical operation.
Between 1980 and 2001, the number of diabetes-related hospital discharges with amputations increased from 33,000 to 82,000 per year. Amputation rates were highest among men, non-Hispanics, blacks and seniors.
In 2003, hospitals discharged 75,000 diabetic patients with amputations. In that year, the amputation rates per 1,000 diabetes was 3.9 among those under age 65, 6.6 among those aged 65 to 74 and 7.9 among those aged 75 years and older.
Federal research shows that 80 percent of non-traumatic amputations start with a foot ulcer, which sets the feet up for infection. The U.S. Department of Health and Human Services’ Behavioral Risk Factor Surveillance Study, or BRFSS, data shows 12 percent of adults with diabetes had a history of foot ulcers, which can lead to amputations.
Research also shows minor trauma, ulcers and poor wound healing leads to 73 percent of foot amputations along with gangrene and infection. Other factors include sensory peripheral neuropathy, changed biomechanics, pressure on the sole of the feet and restricted joint mobility.
Doctors, Specialists Support
To ensure sound foot health, NIDDK, ADA and APMA medical researchers say patient education and overall health self-management are key.
This includes day-to-day foot, eye and oral care, oral exams and medication management. Seniors should also control their blood pressure, blood sugar level and cholesterol and to avoid tobacco or quit smoking to avoid foot troubles, they say.
Federal research finds that 20 percent of diabetics who require routine care will experience a foot care problem that can be treated.
Research also shows that diabetics who smoke are four times more likely than non-diabetic smokers to develop blood vessel disease in the legs. Poor diets and little exercise can contribute to uncontrolled blood sugar and a higher risk of peripheral nervous system and blood vessel diseases.
Additionally, a family history of brain and blood vessel conditions and artery disease may heighten a person’s risk of arterial problems in the legs. Inherited foot shapes may place one in danger of physical deformities leading to skin breakdown.
With the help of their doctors and team of specialists, patients need to follow a healthy lifestyle in which they set realistic goals for losing weight and managing it.
This means watching one’s diet with a variety and balance of healthful carbohydrates or starches, dairy foods, fruits and vegetables and meat or sources of proteins and portion sizes, researchers say.
Seniors must increase fiber and limit saturated fats and salts to control blood sugar, pressure and cholesterol levels. They may recruit a nutritionist as part of their team to help them.
Federal researchers also counsel diabetics to perform moderate daily physical exercise such as walking.
Self-management involves primary care, family practice or internal medicine physicians and specialists advising senior diabetes to point out their greatest concerns.
Doctors and specialists can provide self-management support by asking seniors with diabetes to talk about the goals they would most likely to reach to ensure foot health. They can do so without telling patients what to do to encourage them to make their own decisions.
A medical team can help seniors plan to tackle difficult situations and set practical goals.
Such support could mean, for example, helping a senior plan how to handle a missed medical appointments with his or her doctors or any of his or her specialists.
It could also translate into scheduling such daily activities as dental care, foot care or blood sugar tests and aiding patients in removing barriers to obtaining regular eye exams, foot and oral health exams.
Physicians are asked to consult the National Institutes of Health, or NIH, for guidance on how to discuss foot care self-management at its diabetes care website at http://www.betterdiabetescare.nih.gov/WHATpatientcentereddimensions.htm.
Doctors and specialists ought to ask seniors whether they smoke cigarettes and to urge them to avoid tobacco. Patients can be directed to call the free tobacco hotline at 1-800-QUITNOW.
Seniors who smoke are more likely to develop heart, kidney and eye diseases, stroke, nerve damage and lower extremity conditions, including poor foot health. Diabetics with kidney disease are highly likely to be treated on dialysis. Those on dialysis are at risk of developing foot problems, which, can, however, be treated.
To empower patients to learn more about tobacco cessation or prevention methods, physicians can steer them towards the Center for Disease Control and Prevention’s, or NIH, Tobacco Information and Prevention Source, or TIPS, website at http://www.cdc.gov/tobacco.
They can also ask seniors with diabetes if they know how their disease affects foot health and explain that diabetes can lead to the onset of foot ulcers, which could spell amputation of their limbs. Appropriate foot care is their best defense against such conditions.
Doctors can inquire if seniors have had a complete foot exam, including a sensory exam with a monofilament, in the past year. They can offer to provide an exam and foot inspection or visual foot check or recommend a podiatrist to do so.
If they do test the patient’s feet, doctors or podiatrists can be begin by asking him or her to remove their socks and shoes to check both feet for problems at each visit.
The ADA and the APMA advise that seniors be asked about their regimen of foot care. Those suffering from neuropathy may not see injuries since they don’t feel pain. Doctors can instruct patients to take the following actions to examine their own feet:
- Inspect feet every day by looking and touching;
- Search for cuts, bruises, puncture wounds, swelling, corns or calluses, redness or pus;
- Contact a podiatrist immediately for any of the above foot condition symptoms as they could mean serious injury leading to amputation;
- Keep both the skin and nails of feet clean daily and dry the areas in between the toes;
- Avoid walking barefoot even inside one’s private home, and;
- Wear comfortable and proper footwear such as athletic or walking shoes that fit well and cover feet, not sandals.
Patients most at risk for foot problems ought to prevent ulcers through self-management, foot care and use of proper footwear. The events most likely to cause a foot ulcer are the stubbing of a toe or stepping on a sharp object.
To avoid minor trauma to feet, seniors and their families are asked to clear walking spaces around their private homes, including around the bed and on the way to the bathroom, and to install night-lights.
High-risk seniors must also be aware of who and when to call if they suffer certain foot problems. Patients most at need to call their primary care doctors or podiatrists usually have a puncture wound, ulcer, redness or new foot pain.
Seniors with calluses or thick or ingrown nails are persuaded to contact a podiatrist within a matter of days.
The National Institutes of Health produces literature to educate seniors about proper footcare in both English and Spanish at http://www.ndep.nih.gov/media/feet_broch_eng.pdf.
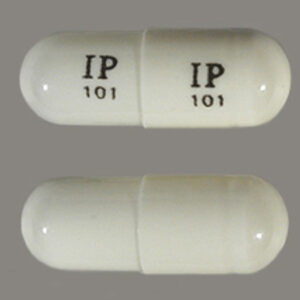
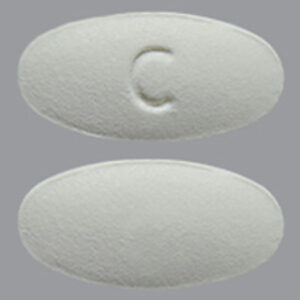
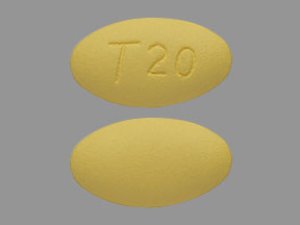
Being a diabetic is hard. Not being able to afford your medications makes it even harder. At Pill Pals, we offer Individual and Employer Sponsored Plans that could benefit Diabetics. Learn more:
Employer Program Features – Pill Pals Pharmacy
For Individuals – Pill Pals Express Pharmacy |
ADDITIONAL SOURCES:
American Academy of Ophthalmology, http://www.aao.org
American Academy of Optometry, http://www.aaopt.org
American Academy of Periodontology, http://www.perio.org
American Association of Clinical Endocrinologists, http://www.aace.com
American Association of Diabetes Educators, http://www.diabeteseducator.org
American College of Clinical Pharmacy, http://www.accp.com
American Dental Association, http://www.ada.org
American Dental Hygienists Association, http://www.adha.org
American Dietetic Association, http://www.eatright.org
American Optometric Association, http://www.aoa.org
American Pharmacists Association, http://www.aphanet.org
American Podiatric Medical Association, http://www.apma.org
American Public Health Association, http://www.apha.org
American Society of Health-System Pharmacists, http://www.ashp.org
HRSA Health Disparities Collaboratives, http://www.healthdisparities.net
National Association of Chain Drug Stores, http://www.nacds.org
National Community Pharmacists Association, http://www.ncpanet.org
National Diabetes Information Clearinghouse, http://diabetes.niddk.nih.gov
National Eye Institute, http://www.nei.nih.gov
National Heart, Lung and Blood Institute, http://www.nhlbi.nih.gov
National Institute of Dental and Craniofacial Research, http://www.nidcr.nih.gov
National Optometric Association, http://www.natoptassoc.org
Photo Credits
https://www.pexels.com/photo/woman-touching-her-right-leg-1204473/